
|
Navin K. Kapur, MDCertificationsExecutive Director, The CardioVascular Center for Research and Innovation (CVCRI); Director, Acute Mechanical Circulatory Support Program; Director, Interventional Research Laboratories; Director of Cardiac Biology Research Center, Molecular Cardiology Research Institute (MCRI); Associate Professor University / Hospital AffiliationTufts University School of Medicine AboutDr. Kapur is a dual, board-certified Interventional Cardiologist and Advanced Heart Failure/Cardiac Transplant specialist. He is Director of the Acute Circulatory Support Program and Associate Director of the Cardiac Catheterization Laboratory at Tufts Medical Center. His clinical expertise focuses on invasive hemodynamics, mechanical circulatory support, and interventional therapies for patients with advanced heart failure. He serves on several national committees involved with the American Heart Association, the American College of Cardiology, the Heart Failure Society of America, and the Society for Cardiac Angiography and Interventions.
As Director of the Interventional Research Laboratories at Tufts Medical , Dr. Kapur’s translational research focuses on large animal models of acute and chronic heart failure, circulatory support device development, and cardioprotective mechanisms in the setting of acute myocardial infarction. His recent work has focused on the hypothesis that mechanically unloading the heart and delaying coronary reperfusion limits infarct size. This concept known as the 'mechanical conditioning hypothesis' has the potential to alter the paradigm of acute heart attack therapy and reduce the burden of ischemic heart failure.
As Director of the Cardiac Biology Research Center within the Molecular Cardiology Research Institute at Tufts Medical Center, Dr. Kapur’s basic science laboratory focuses on molecular mechanisms governing maladaptive cardiac remodeling in heart failure. His particular expertise involves signaling via the transforming growth factor beta (TGFb) system. Over the past 6 years, the laboratory has published several critical papers focused on a TGFb co-receptor known as endoglin and was the first to establish that reduced endoglin activity improves survival and limits maladaptive cardiac remodeling in heart failure. More recently, the laboratory has demonstrated that targeting endoglin using an antibody-mediated approach not only limits the development of cardiac fibrosis, but can reverse established cardiac fibrosis in preclinical models of heart failure. Dr. Kapur is the recipient of grant funding from the National Institutes of Health, American Heart Association, and several industry sponsors.
|
Related Content
 video Machine Learning Mortality Prediction for Patients with Cardiogenic Shock due to Acute Decompensated Heart FailureDiscussion leaders: Prof. Dr. Med. Bart Meyns (KU Leuven, Belgium) and Kiyotake Ishikawa, MD, PhD (Mount Sinai, USA)
Speaker: Navin... |  Pecha Kuchavideo Pecha Kucha: Can Mechanical Preload Reduction benefit PatientsModerators: Navin Kapur, MD (Tufts Medical Center, USA) and Dan Burkhoff, MD, PhD (Cardiovascular Research Foundation,... | 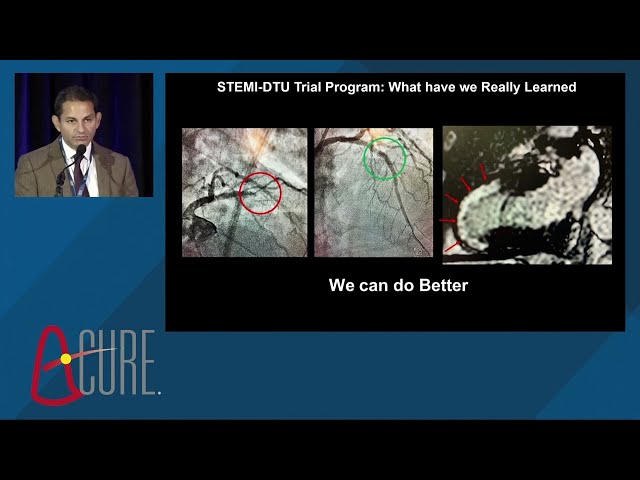 video Delaying Reperfusion for Thirty Minutes in the Presence of Active LV Unloading Reduces Infarct Size in Anterior...Navin Kapur, MD (Tufts Medical Center) presents Delaying Reperfusion for Thirty Minutes in the Presence of Active LV Unloading Reduces... |
Manuscripts & Publications
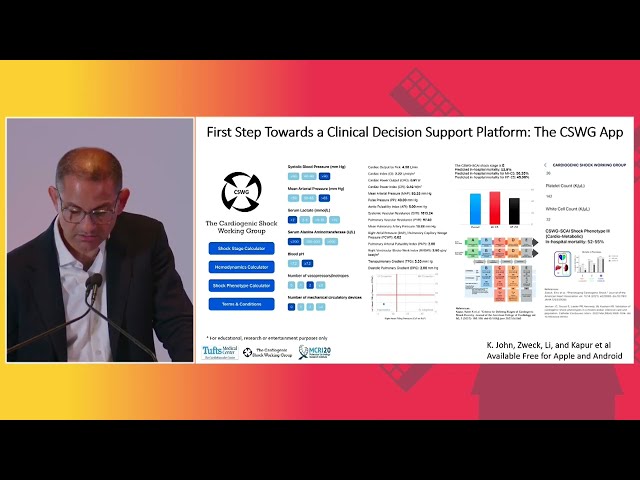
SCAI SHOCK Stage Classification Expert Consensus Update: A Review and Incorporation of Validation StudiesSince its development and release in 2019, the Society for Cardiovascular Angiography and Interventions (SCAI) shock stage classification for adult patients has been widely cited and increasingly incorporated, owing to its simplicity across all clinical settings, easily understood and visualized framework, and notable endorsement by relevant societies and organizations that manage cardiogenic shock (CS).
|
|
Escalating and De-escalating Temporary Mechanical Circulatory Support in Cardiogenic Shock: A Scientific Statement From the American Heart AssociationThe use of temporary mechanical circulatory support in cardiogenic shock has increased dramatically despite a lack of randomized controlled trials or evidence guiding clinical decision-making. Recommendations from professional societies on temporary mechanical circulatory support escalation and de-escalation are limited.
|
|
Mechanical Left Ventricular Unloading in Patients Undergoing Venoarterial Extracorporeal Membrane OxygenationVenoarterial extracorporeal membrane oxygenation (VA-ECMO) increases left ventricular (LV) afterload, potentially provoking LV distention and impairing recovery. LV mechanical unloading (MU) with intra-aortic balloon pump (IABP) or percutaneous ventricular assist device (pVAD) can prevent LV distension, potentially at the risk of more complications, and net clinical benefit remains uncertain.
|